Working Diagnosis:
Hypertrophic cardiomyopathy with pathogenic variant in MYBPCS c.1244-52 G>A. His mother was also genotype positive/phenotype negative. His father and siblings were both genotype and phenotype negative. Extended family members were contacted and opted for no further testing.
Treatment:
The athlete's European Society of Cardiology-Hypertrophic Cardiomyopathy (ESC-HCM) five year SCD risk was calculated to be low (3.31%) and implantable cardioverter-defibrillator placement was not indicated. The patient was asymptomatic and thus pharmacologic treatment as also not recommended. Shared decision making per the 2020 AHA guidelines was conducted between the patient, his parents, his HCM cardiology team, school athletic director, team physicians, and athletic trainers.
Outcome:
The athlete's symptoms resolved on the same day that he presented to the primary care physician and have not returned. Decision made to allow the athlete to return to full participation with an emergency action plan. This athlete fully participated in the 2021 football season without symptoms or event. His emergency action plan includes BLS-trained coaches, personal AED, and EMS at games. His annual HCM cardiology screening includes cardiac MRI, two-week ambulatory cardiac monitor, and a maximal stress echocardiogram, and cardiopulmonary exercise testing to assess for disease progression.
Author's Comments:
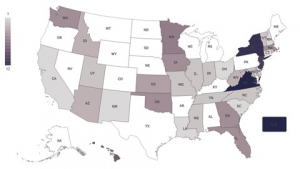
Hypertrophic cardiomyopathy (HCM) is the most common cause of sudden cardiac death (SCD) in young athletes with increased risk for black, male football players (Baggish et al, 2020). Echocardiogram is the gold-standard imaging modality to diagnose HCM, however, cardiac MRI findings may play an increasing role in HCM risk stratification. HCM is diagnosed by Z score >2 in children or septal wall thickness >15mm in adults (Baggish et al, 2020). This athlete's Z score on echocardiogram was not diagnostic for HCM, yet his cardiac MRI and genetic testing clearly confirm his diagnosis of familial HCM.
Guidelines for sports participation in athletes with SCD-associated cardiovascular conditions, such as hypertrophic cardiomyopathy, have evolved from blanket disqualification in 2005 to exceptions for Class 1A sports in 2015 (Maron et al, 2015). Current recommendation is to consider discussion of the treatment options, potential harms, and benefits of continued sports participation and patient values within a shared decision-making model (Drezner et al, 2020). The 2020 ACC/AHA guidelines now include a Class 1 indication for moderate intensity recreational exercise of 150-300 minutes per week based on RESET-HCM trail published in JAMA in March 2017 (Ommen, et al., 2020; Saberi et al, 2017). There continues to remain some uncertainty, however, regarding participation in vigorous exercise and competitive sports such as football leading to a Class 2b, LOE C recommendation (Ommen, et al., 2020). There is limited prospective cohort data (n=88) showing no difference in the risk of sudden cardiac arrest for adults with low-risk HCM phenotype who continued to participate in intensive sports over 7-year period compared to those that did not participate (Pelliccia, et al., 2020). This data, however, may not apply to younger or adolescent athletes or those with more severe HCM phenotype where risk of sudden cardiac death may be higher but is still unknown. The larger powered LIVE-HCM trial (n=~1800) which is currently in data analysis and includes younger adolescent athletes may prove enlightening for future cases.
This athlete did not have any conventional risk factors of sudden cardiac death to include: no prior cardiac arrest, family history of HCM-related sudden cardiac death, unexplained recent syncope, multiple episodes of non-sustained ventricular tachycardia, wall thickness ≥ 30 mm, LV apical aneurysm, EF 50mmHg (Maron, 2018). His ESC-HCM was noted to be 3.31%, less than 4% which is the cutoff at which an internal cardiac defibrillator is typically considered (Elliott et al., 2014). Variables considered in ESC-HCM score calculation include age (must be >16 years old), maximal LV wall thickness, left atrial size, LVOT gradient, family history of SCD, non-sustained ventricular tachycardia, and unexplained syncope.
The athlete's ESC-HCM score, lack of conventional SCD risk factors, and uncertainty of whether participation in competitive sports or vigorous recreational exercise increases the risk of SCD or arrhythmia beyond the baseline risk for young athlete with HCM were discussed with all pertinent parties. There was consensus among all parties to allow the athlete to fully participate in the 2021 football season.
Editor's Comments:
This case highlights individualized shared decision making between the athlete, family, HCM cardiologist,
and third parties (coach, school, ATC, head team physician) rather than blanket disqualification for athletes with HCM. In the US, legal precedent supports that high school students with heart disease have no compelling right to participate in interscholastic sports without medical clearance and that college athletes with life-threatening cardiac conditions can be medically disqualified and eligibility decisions reside with the team physician. Therefore, it is important for the team physician to be aware that eligibility decisions may be influenced by the policies and laws dictated by the relevant country or sports governing body.
References:
2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy." European Heart Journal 35 (2014): 2733-2779.
Baggish, Aaron L., et al. "Recommendations on the use of multimodality cardiovascular imaging in young adult competitive athletes: a report from the American Society of Echocardiography in Collaboration with the Society of Cardiovascular Computed Tomography and the Society for Cardiovascular Magnetic Resonance." Journal of the American Society of Echocardiography 33.5 (2020): 523-549.
Drezner, Jonathan A., et al. "Return to play with hypertrophic cardiomyopathy: are we moving too fast? A critical review." British journal of sports medicine 55.18 (2021): 1041-1047.
Maron, Barry J., Douglas P. Zipes, and Richard J. Kovacs. "Eligibility and disqualification recommendations for competitive athletes with cardiovascular abnormalities: preamble, principles, and general considerations: a scientific statement from the American Heart Association and American College of Cardiology." Journal of the American College of Cardiology 66.21 (2015): 2343-2349.
Maron, Barry J. Clinical course and management of hypertrophic cardiomyopathy. N Engl J Med (2018); 379: 655-68.
Ommen, Steve R., et al. "2020 AHA/ACC guideline for the diagnosis and treatment of patients with hypertrophic cardiomyopathy: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines." Journal of the American College of Cardiology 76.25 (2020): e159-e240.
Pelliccia A, Caselli S, Pelliccia M. et al. Clinical outcomes in adult athletes with hypertrophic cardiomyopathy: a 7-year follow-up study. Br J Sports Med. 2020; 54: 1008-12.
Sharma, Sanjay, et al. "International recommendations for electrocardiographic interpretation in athletes." Journal of the American College of Cardiology 69.8 (2017): 1057-1075.
Return To The Case Studies List.