COLLABORATIVE SOLUTIONS FOR SAFETY IN SPORT:
A CALL TO ACTION TO ENSURE BEST PRACTICES ARE IN PLACE IN SECONDARY SCHOOL SPORTS
Establishment of Emergency Action Plans a Primary Focus
NEW YORK CITY, March 26, 2015 – Nearly all deaths and serious injuries that have long-term complications can be avoided when proper steps are taken to prevent, recognize and treat the major medical conditions that a high school athlete may experience during practices and competitions.
This was the collective message of national sports medicine leaders today during a national press event at the NFL headquarters and hosted by the National Athletic Trainers’ Association (NATA) and American Medical Society for Sports Medicine (AMSSM). The experts encouraged the establishment of best practices and protocols with regard to heat-related illnesses, cardiac conditions, head and neck injuries and the overarching need for emergency action plans (EAPs) in all high schools.
This message was also reinforced in a Journal of Athletic Training editorial, “Moving Forward Faster: The Quest to Apply Evidence-Based Emergency practice Guidelines in High School Sports.” The editorial was released online this morning in the Journal, NATA’s scientific publication, http://natajournals.org/doi/pdf/10.4085/1062-6050-50.4.01.
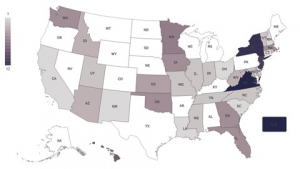
In 2014, more than 15 high school athletes lost their lives during sports or physical activity. Thousands more develop acute or long-term injuries as a result of participation. Today, only 22 percent of states meet the recommendation that every school or organization that sponsors athletics develop an EAP for managing serious and or potentially life-threatening injuries. Fourteen out of 50 states currently meet the minimum best practices with regard to heat acclimatization. Only 50 percent of states have met recommendations that all athletic trainers, coaches, administrators, school nurses and others have access to an automated external defibrillator.
While the National Federation of State High School Associations oversees state associations and provides recommendations, it does not have the authority to direct states on their individual protocols. As a result, life-saving health policies are implemented state by state. In 2013, an Inter-Association Task Force for Preventing Sudden Death in Secondary School Athletics Programs: Best Practice Recommendations” was published in the Journal of Athletic Training. Fourteen sport and health associations endorsed the statement. These guidelines serve as a cornerstone for today’s event.
Following the press conference, NATA and AMSSM with the support of the Korey Stringer Institute and the NFL, will bring together key stakeholders in high school athletics to discuss these recommendations. Leaders from all 50 states will be in attendance and will represent sports medicine advisory committees, high school activity associations and high school athletic associations. The goal is for all state high school associations to adopt guidelines and specifically the establishment of emergency action plans.
“The National Athletic Trainers’ Association remains committed to the health and welfare of student athletes,” says Jim Thornton, MA, ATC, CES, NATA president. “We, along with AMSSM continue to champion best practices and the presence of the appropriate sports medicine professionals on the field during practices and games to ensure safety. Currently, only 37 percent of high schools across the country have full-time athletic trainers, and athletic trainers play a key role in implementing and ensuring adherence to these best practices.”
“The American Medical Society for Sports Medicine shares NATA’s commitment,” says President Christopher Madden, MD. “Our goal today is to develop a collaborative forum to share resources, tools, best practices and strategies designed to advance the safety of student athletes in secondary schools.”
Nationally Acclaimed Speakers Address Secondary School Health and Safety Protocols
The press conference included prominent youth sports safety medical experts. Thornton and Madden opened the program. Douglas Casa, PhD, ATC, FNATA, chief operating officer, Korey Stringer Institute, and director of Athletic Training Education and professor in the Department of Kinesiology at the University of Connecticut addressed exertional heat stroke; Jason Cates, ATC, LAT, member, Arkansas Activities Association Sports Medicine Advisory Committee; head athletic trainer, Cabot Public Schools; past president, Arkansas Athletic Trainers’ Association discussed advancements in Arkansas youth sports safety state policies and guidelines and specifically the passage of a law in 2011 requiring emergency action plans for all athletic venues, practices and games. Jonathan Drezner, MD, professor in the department of family medicine at the University of Washington; team physician for the Seattle Seahawks and the University of Washington Huskies; and director of the UW Medicine Center for Sports Cardiology talked about cardiac conditions and the critical need for emergency action planning; Kevin Guskiewicz, PhD, ATC, FNATA, Kenan Distinguished Professor and founding director of the Matthew Gfeller Sport-Related Traumatic Brain Injury Research Center and Center for the Study of Retired Athletes, University of North Carolina, Chapel Hill addressed head and neck Injuries. Roman Oben, director, youth and high school football, National Football League and former NFL player provided insight on playing it safe with best practices in place and reviewed many of the current policies and programs the league has established.
Recommendations for Evidence-Based Best Practices in High School Sports
In an effort to provide coaches, athletic directors, parents, athletes, school administrators and others with health and safety best practices, the sports medicine experts provided the following recommendations:
1. Create an emergency action plan in collaboration with coaches, athletic trainers, other medical professionals and local and campus safety officials.
2. Have athletic trainers on staff: athletic trainers play a critical role in preventing sudden death in sport such as prevention, diagnosis, emergency care and treatment.
3. Acquire and place automated external defibrillators (AEDs) on school campuses and at sporting facilities for immediate access in the case of a cardiac emergency.
4. Ensure that athletes acclimatize progressively to training demands and environmental conditions for optimal safety. Conditioning should be phased in gradually: the first seven to 10 days of any new cycle should be considered transitional. Exercise and conditioning should not be used as punishment.
Emergency Action Plans
1. Every school should develop an EAP for managing serious and or potentially life-threatening injuries. It should be site-specific and include maps and/or specific direction to that venue.
2. The EAP should be reviewed each season and updated as necessary.
3. The plan should be developed and coordinated with local EMS, venue public safety officials, on-site medical personnel or organization administrators. It should be a written document distributed to all staff members.
4. Each school should post the location of all emergency equipment and provide a readiness check before each scheduled athletic activity. This includes AEDs which should be strategically located to allow immediate retrieval and use within three minutes of recognizing an emergency.
5. The EAP should identify personnel and their responsibilities to carry out the plan of action with a designated chain of command. Health care professionals who will provide medical coverage during games, practices or other events should be included.
Catastrophic Brain and Neck Injuries
- Concussions remain a clinical diagnosis ideally made by a health care provider (team physician and athletic trainer) familiar with the athlete and knowledgeable in the recognition and evaluation of concussion. A comprehensive, standardized assessment tool should be included in the evaluation.
- An annual brain and spine safety education program, and in-season behavior modification “check-ups” should be conducted for all student athletes. Be cognizant of athletes’ medical conditions.
- Athletic trainers and school officials should enforce the standard use of certified helmets.
- A comprehensive medical-management plan for acute care of potential spine or brain injury should be implemented if the patient has altered levels of consciousness, substantial neurologic concerns, midline spine pain or obvious spinal column deformity.
- The athletic trainer and team/treating physician should work together to implement a gradual return to participation progression for the concussed athlete. No secondary school athlete with a suspected concussion should be permitted to return to practice, game or activity on the same day; and should follow a supervised six-step gradual return from no activity to light, sport-specific, non-contact, limited and then full return to participation. The patient should also receive a written release from a medical professional trained in concussion evaluation and management.
Exertional Heat Stroke (EHS)
- Before the season begins, all teams should follow a heat acclimatization program that focuses on phasing in equipment use, intensity and duration of exercise and total practice time.
- Administrators, coaches, athletes and parents must be educated about common causes and risk factors of heat stroke.
- Activities should be modified when environmental conditions are extreme.
- Water or sports drinks must be available and placed at key locations on the field for players to drink quickly and freely during practice, conditioning sessions and competitions.
- Exertional heat stroke should be suspected in any athlete who exhibits extreme hyperthermia and central nervous system dysfunction during exercise in the heat. If EHS is suspected, a rectal temperature reading by an athletic trainer or physician is recommended to verify the diagnosis. If EHS is present, cold-water immersion should be implemented immediately and completed before transport. All schools should have a cold water immersion tub, and all patients with EHS should be monitored thoroughly for return to play considerations and cleared by a physician.
Sudden Cardiac Arrest (SCA)
- Athletes should undergo cardiovascular screenings before participation in competitive activities.
- An automated external defibrillator (AED) should be on-site and readily available within three minutes (with one minute being ideal) for all organized sports activities.
- School staff, medical professionals, coaches and athletes should be educated annually about location and use of AEDs.
- Any athlete who has collapsed and is unresponsive should be assumed to be in SCA until proven otherwise.
- Proper management includes: prompt recognition of SCA (brief seizure-like activity occurs in 50 percent of young athletes with SCA and should not be mistaken for a seizure); early activation of the EMS system (call 9-1-1); early CPR beginning with chest compressions; early use of an AED; and transport of the patient with SCA to a hospital capable of advanced cardiac care.
“This morning’s event provides clear guidelines for all of us to consider when shaping state high school sports safety protocols,” said Thornton. “Adopting these measures and putting them into practice will potentially help save lives and reduce injury. These recommendations are vital and reinforce our commitment to safety today.”
“Our collaborative approach to high school sports safety is a true team approach. We encourage all of those in attendance and who touch the lives of young athletes to review, consider and implement these best practices,” added Madden. “Each organization, each state athletic association has a critical role to protect these athletes and help them succeed in sport and life.”
Speaker information or interviews are available upon request. For more information on each of the topics mentioned, please visit: www.SolutionsForAthleteCare.org
About AMSSM: American Medical Society for Sports Medicine (AMSSM) is a multi-disciplinary organization of 2,700+ sports medicine physicians dedicated to education, research, advocacy and the care of athletes of all ages. The majority of AMSSM members are primary care physicians with fellowship training and added qualification in sports medicine who then combine their practice of sports medicine with their primary specialty. AMSSM includes members who specialize solely in non-surgical sports medicine and serve as team physicians at the youth level, NCAA, NFL, MLB, NBA, WNBA, MLS and NHL, as well as with Olympic teams. By nature of their training and experience, sports medicine physicians are ideally suited to provide comprehensive medical care for athletes, sports teams or active individuals who are simply looking to maintain a healthy lifestyle. Visit www.amssm.org
About NATA: National Athletic Trainers’ Association (NATA) – Health Care for Life & Sport
Athletic trainers are health care professionals who specialize in the prevention, diagnosis, treatment and rehabilitation of injuries and sport-related illnesses. They prevent and treat chronic musculoskeletal injuries from sports, physical and occupational activity, and provide care for acute injuries. Athletic trainers offer a continuum of care that is unparalleled in health care. The National Athletic Trainers’ Association represents and supports 39,000 members of the athletic training profession. Visit www.nata.org
# # #